Alexander D. Horsch
Our study was part of the prospective multicenter Dutch acute stroke study (DUST), which was funded by the Netherlands Heart Foundation in collaboration with the MR CLEAN study, and received additional funding from the Nuts Ohra Foundation. The main aim of DUST was to investigate the use of advanced CT imaging (CTP and CTA) in outcome prediction in patients with acute ischemic stroke.1
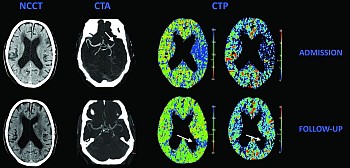
The treatment of ischemic stroke has changed greatly over the last 20 years, first with the emergence of thrombolysis (IV-rtPA) and, more recently, with the addition of intra-arterial thrombectomy (IAT).2 Both treatments aim to resolve the obstructing clot. In a recent consensus meeting (Acute Stroke Imaging Research Roadmap II) it was suggested that revascularization is a combination of 3 mechanisms: recanalization (obtaining arterial patency at the location of the primary occlusion), reperfusion (antegrade microvascular perfusion), and collateralization (microvascular perfusion via pial arteries or other anastomotic channels that bypass the primary occlusion).3 All 3 parameters can be evaluated with advanced CT imaging. In many articles recanalization has been considered to be synonymous with reperfusion, but other articles suggest that reperfusion is a better predictor of final infarct volume and clinical outcome.4 In this study we evaluated the relationship between reperfusion and recanalization, and investigated which clinical and imaging parameters predict complete reperfusion in a population considered for treatment with IV-rtPA only.