Joshua Nickerson
Brain perfusion imaging using MR is not a new idea, and indeed, both gadolinium-based techniques and noncontrast methods have been well described in the radiology literature for decades. However, in discussion with colleagues, both in academia and in the private practice world, it is apparent that, currently, dynamic perfusion scanning has become part of the routine clinical examination at only a few of the largest centers in the United States. Reasons range from lack of experience, poor postprocessing software, limited display capabilities of PACS, lack of quantification, and confusion over the utility of the information obtained. Nevertheless, DSC and dynamic contrast-enhanced (DCE) sequences have been available commercially from MR vendors for some time and have found a role in some centers for evaluation of tumor, stroke, seizure, and myriad other conditions.
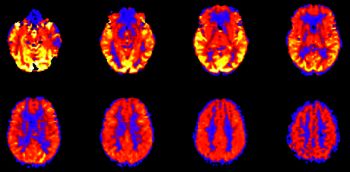
Arterial spin-labeled (ASL) perfusion imaging has also been around for quite a while, but until recently has been largely confined to the research realm. However, advances in data acquisition techniques, MRI technology, and processing software have resulted in the inclusion of ASL sequences in the armamentarium prepackaged by the major MR vendors. ASL has a number of advantages over gadolinium-based methods, including (obviously) the lack of contrast, which allows for short-term repeatability and, also, at least a semi-quantitative measure of cerebral blood flow depending on the technique used. Admittedly, there are disadvantages, including a relatively limited signal-to-noise ratio and as of yet cumbersome postprocessing needed for quantification. But particularly as the latter concern is progressively overcome by software vendors, we may begin to see this technology find more and more applications in the near future—a contrast-free sequence yielding whole-brain perfusion maps that only takes on the order of 3–4 minutes has undeniable appeal!