Autoimmune encephalitis (AE) is an increasingly recognized category of antibody-mediated CNS disease that can have a wide range of clinical manifestations based on the specific brain regions involved. While clinical AE phenotypes of limbic dysfunction and/or seizure were the first to be recognized, it is now understood that a growing list of pathologic AE antibodies can result in other forms of neurologic impairment such as dysautonomia, ataxia, bulbar palsy, movement disorders, psychosis, and progressive cognitive decline. This is a challenging diagnosis to make prospectively given the diverse spectrum of clinical phenotypes and the ability to mimic many other disease processes, but early diagnosis and treatment should be the goal as it is consistently associated with improved clinical outcomes. Adequate treatment of patients with AE may require identification and treatment of an underlying systemic malignancy or may require long-term immunomodulatory therapy to prevent relapse in patients with purely autoimmune forms of the disease.
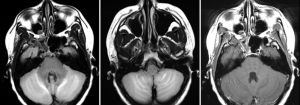
Neuroimaging plays a crucial role in the work-up of these patients, initially by excluding other more common causes of neurologic impairment, but it is also being used in research to identify characteristic imaging findings and to better understand the underlying pathophysiology. Our initial effort to provide a comprehensive literature review of AE neuroimaging findings has led to an ongoing collaboration to better characterize the various neuroanatomic patterns of disease that can be seen when imaging the brain, optic nerves, and spinal cord in any number of antibody-mediated CNS conditions, such as those targeting components of the neuronal synapse (AE), axons/myelin (GQ1b, MOG), and astrocytes (AQP4, GFAP).