Mahmud Mossa-Basha
Extracranial carotid vulnerable plaque imaging is a maturing field in both the clinical and research realms, providing information that goes beyond standard luminal imaging techniques. The North American Symptomatic Carotid Endarterectomy Trial and the European Carotid Surgery Trial have formed the basis of reliance on carotid luminal stenosis measurements to determine the risk for future stroke events and the need for surgical intervention. The degree of luminal narrowing, however, is not the only determining factor for stroke risk. Factors such as plaque composition and morphology, independent of their hemodynamic effect on the lumen, have been shown to contribute to the risk of plaque rupture and future cerebrovascular events. Some of the factors that contribute to vulnerable atherosclerotic plaque include prominent lipid necrotic cores, fibrous cap rupture, intraplaque hemorrhage, plaque inflammation, ulceration, and neovascularity.
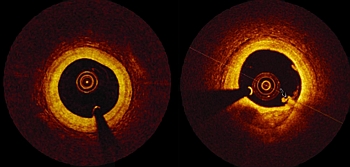
Cross-sectional imaging, including MRI and CT, has been extensively studied to determine its ability to identify vulnerable plaque characteristics. MRI carotid vulnerable plaque imaging has contributed significantly to plaque imaging and characterization over the past 10–15 years. MR imaging is emerging as the best technique to assess for high-risk plaque features that can affect patient management. CT angiography has also proven adept at detecting atherosclerotic plaque irregularities and ulcerations, as well as prominent lipid necrotic cores and plaque calcification.
The University of Washington Vascular Imaging Lab has been at the forefront of carotid MRI vulnerable plaque imaging research, and these techniques have now been translated to the clinical realm. Plaque imaging can uncover the presence of fibrous cap rupture and vulnerable plaque characteristics that could lead to rupture, in patients with cryptogenic stroke and TIA. This can modify treatment and potentially result in surgical intervention in a patient who otherwise would have been managed by conservative therapy under current guidelines. Larger multicenter prospective trials—investigating the use of carotid MRI vessel wall imaging