Approximately 4.3 million (1.8%) adults and 750,000 (1.0%) children in the United States have been diagnosed with epilepsy or other seizure disorders; approximately one-third have seizures refractory to medical therapies.1,2 MRI is essential for the assessment of these patients with medically refractory epilepsy, as it allows identification of structural abnormalities which, when resected, may lead to seizure freedom. Task-based functional MRI (fMRI) has been shown to aid structural MRI in the evaluation of epilepsy by determining the relationship between epileptogenic lesions and the normal brain. It is being used more frequently in the presurgical evaluation of these patients, including the localization of motor and language function. Recently, several studies have used resting-state functional MRI (rs-fMRI) to describe cortical network alterations in patients with epilepsy.
Briefly, blood oxygen level–dependent (BOLD) fMRI detects neural activity by imaging changes in local oxygen metabolism in the brain. fMRI contrast relies on the different magnetic properties between diamagnetic oxygenated (HbO) and paramagnetic deoxygenated hemoglobin (HbR). During task-based fMRI, neural activity in the parts of the brain involved in performing the task causes a localized increase in oxygen consumption. However, cerebral blood flow increases within seconds, creating a surplus of HbO in these same regions. This results in an overall decrease in regional HbR concentration, a decrease in susceptibility effects, and an increase in the measured T2* BOLD signal.
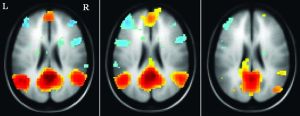
Conversely, rs-fMRI evaluates the brain in the absence of a stimulus (or at rest) and studies synchronous fluctuations in the BOLD response between areas of the brain that are spatially separated to identify resting-state networks (RSNs). Conceptually, these spontaneous but synchronous fluctuations in the BOLD signal are thought to reflect the underlying functional architecture of the brain; collections of regions with correlated spontaneous BOLD fluctuations represent networks of anatomically distinct areas that nevertheless work together to perform a common function. These RSNs were described in positron-emission tomography and electroencephalography studies in the 1980s. In 1995, Biswal et al3 were the first to use resting-state fMRI to describe functional connectivity between the sensorimotor cortex of the two cerebral hemispheres. The best described RSN is the default mode network (DMN), which comprises multiple regions—or “nodes”—within the posterior cingulate cortex, as well as the medial temporal and medial prefrontal lobes.4 Aberrations in connectivity strength across the DMN have since been implicated in multiple mental disorders, including schizophrenia, Alzheimer disease, and depression.4
This AJNR News Digest highlights five rs-fMRI studies in patients with epilepsy that contribute to our understanding of the pathogenesis of seizure disorders and show the potential for monitoring and observing injuries in these patients.