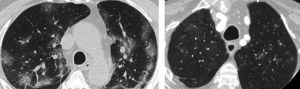
At the very start of the pandemic, when performing emergency CTA for patients with suspected stroke, we noticed the presence of ground-glass opacification (GGO) in the apices in those with COVID-19. Additionally, we were aware that the results for Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) reverse-transcriptase polymerase chain reaction (RT-PCR) testing were not ready until hours after the CTA, which occurred immediately on admission. If proven, we suspected the presence of GGO would be a simple and “opportunistic” diagnostic biomarker available prior to the PCR results. That had major implications for the management of patients with suspected stroke through early identification of COVID-19 and the limitation of disease transmission.
Therefore, we evaluated the reliability and accuracy of all candidate diagnostic imaging biomarkers. Similarly, we analyzed all the nonimaging “opportunistic” information such as demographics, clinical features, and risk factors for COVID-19 and stroke using univariate and multivariate statistics.
The results show that when the researchers saw these changes in the top of the lungs during the emergency scan, they were able to reliably and accurately diagnose COVID-19, and the changes also predicted increased mortality. This is particularly relevant given the limitations of currently available SARS-CoV-2 RT-PCR testing, as it takes time to complete the test and sometimes it is inaccurate.
The findings can allow earlier selection of the appropriate level of personal protective equipment and attendant staff numbers, triage to appropriate inpatient ward settings, self-isolation, and contact tracing. Additionally, our data have prognostic information given the increased mortality in those with lung changes shown in our cohort.
These are useful results because the changes are simple for radiologists and other doctors to see. This is “free information” from a scan intended for another purpose, yet it is extremely valuable.
The work has been well received, highlighted in news outlets, and spread on social media in Europe and the Americas.