The discovery of CSF venous fistulas (CVFs) as a cause of spontaneous intracranial hypotension (SIH) has had a profound impact on treatment.1 Patients with no visible epidural fluid leakage who were once thought to have slow-flow leaks are increasingly recognized as harboring CVFs. The diagnosis of CVF is important because these patients do not respond well to epidural blood patches and usually require surgery to cure.2,3
CVFs can be quite difficult to find in some patients, however. Once initial spine imaging is performed and found to show no epidural fluid, some authors advocate for digital subtraction myelography (DSM) performed in the decubitus position.4 This technique requires 2 procedures on subsequent days, both requiring general anesthesia. Alternative methods of identifying CVFs are therefore clearly desirable.
CT myelography is performed at some institutions as initial spine imaging and has the advantage of being capable of detecting both epidural fluid and CVFs.5 Improving CVF detection on CT myelography would obviate the need for subsequent DSM.
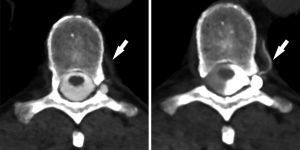
In this article, we report on our experience that simply turning a patient to the decubitus position greatly facilitated the diagnosis in some cases. This effect seems to be partly due to increased contrast density over a fistula site due to dependent layering of intrathecal contrast, but also seems to be due to gravitational effects that promote filling of the fistula in the decubitus position.