Asim Choudhri
Diffusion-weighted imaging rose to prominence due to its ability to rapidly detect early signs of cellular metabolic shutdown (cytotoxic edema), and it quickly became the gold standard for the detection of acute cerebral infarction. While DWI is typically evaluated in a qualitative manner, quantified calibrated information can be obtained in the form of apparent diffusion coefficient maps. Further advances in quantification of the direction of motion in diffusion tensor imaging have allowed an important tool for mapping white matter pathways. More recent work evaluating the non-Gaussian properties of water diffusion has resulted in diffusion kurtosis imaging (DKI). Simultaneous with these advances in technology has come a greater appreciation for the information contained in the original diffusion-weighted sequence.
The nuclear-to-cytoplasmic ratio of a tumor tends to correspond to tumor cellularity and grade. To a first approximation, using a rudimentary understanding of histopathology (which is the extent of my knowledge), more purple and less pink on an H&E slide corresponds with more aggressive tumors. Pink areas on H&E correspond to cytoplasm, which has relative facilitated diffusion, and purple areas correspond to the nucleus, which is densely packed and thus has less free water diffusion. Accordingly, a high nuclear-to-cytoplasmic ratio will tend to be associated with reduction in the free diffusion of water molecules as depicted by low ADC values. In this issue of AJNR Digest, we have focused on important articles that use ADC values to attempt to stratify tumor histopathology.
In the article by Rumboldt et al,1 ADC values were evaluated in 32 children with posterior fossa masses. There were statistically differing groupings of ADC values between pilocytic astrocytomas (WHO grade I), ependymoma (WHO grade II), and medulloblastoma (WHO grade IV). On a patient-basis, the pilocytic astrocytoma with the lowest ADC was similar to the ependymoma with the highest ADC. Similarly, the ependymoma with the lowest ADC was similar to the medulloblastoma with the highest ADC. While this was a small series, and there were no anaplastic ependymomas, this important article helped pave the way for diffusion to stratify tumor histology.
Kralik et al2 expanded upon the use of ADC to characterize tumors in 19 children presenting with supratentorial tumors in the first year of life. Given the heterogeneity of histopathologic diagnoses in this group, the authors performed a correlation study between ADC and tumor grade instead of comparing by diagnosis, confirming a negative correlation (ie, low ADC corresponded to high tumor grade).
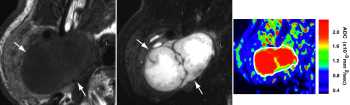
Toh et al3 applied these techniques to infiltrating cerebral neoplasms in adults, in particular lymphoma and glioblastoma, two entities that are commonly stated to be relatively indistinguishable. ADC values in lymphoma were shown to be lower than those of glioblastoma. Fractional anisotropy was also shown to be lower in lymphoma than glioblastoma in this study that used diffusion tensor imaging.
Dumrongpisutikul et al4 compared ADC values in 20 pineal cell tumors spanning all age groups and showed pineal cell origin tumors had lower ADC values than germinomas. This has significant implications, as germinomas are typically treated by adjunctive therapy as opposed to maximal cytoreductive surgery.