Guest Editor
Hillary R. Kelly
Minimally invasive parathyroidectomy (MIP) has increasingly become the standard of care for surgical treatment of primary hyperparathyroidism over bilateral neck exploration, due decreased morbidity and costs, with similar rates of surgical cure.1–3 Precise and accurate preoperative localization is critical to the successful performance of MIP, and parathyroid imaging has gone through a series of changes and innovation as a result. Cross-sectional imaging has much to offer this patient population. In this issue of the AJNR News Digest, we highlight the emerging techniques of dynamic contrast-enhanced CT and MR imaging for preoperative localization of parathyroid lesions.
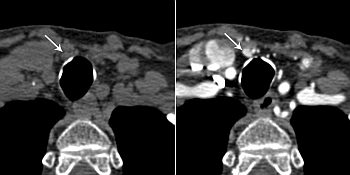
Multiphase multidetector CT for localization of parathyroid adenomas and multigland hyperplasia is also known as 4D-CT (4-dimensional CT), referring to the combination of multiplanar “3-dimensional CT” and the added fourth “dimension” derived from changes in enhancement over time.4 Although the vast majority of the literature has focused on 4D-CT4–11, a few recent studies have outlined a similar approach using MRI.12–14
4D-CT was first described in the surgical literature in 2006,4 and multiple subsequent studies have reported higher sensitivity and accuracy relative to the traditional imaging modalities of technetium Tc99m sestamibi and ultrasonography.5,6,9,15,16 However, there remains wide variability in the technical protocols used at various institutions10 and significant concerns regarding radiation exposure.5,9,10,17,18
There is persistent controversy over the optimum number of phases for 4D-CT. The original protocol included 4 phases: non-contrast-enhanced and 3 contrast-enhanced phases (arterial and 2 delayed venous phases).4 A few of the largest retrospective studies reported similar or improved sensitivities and accuracies for 3-phase protocols (noncontrast, arterial, and 1 delayed phase) compared with 4-phase 4D-CT and/or scintigraphy16 (AJNR 2014;35:176–18). Subsequently, a few papers have argued for 2 or fewer phases,19 including 2 of the articles selected for this issue (AJNR 2014;35:1959–64, AJNR 2015;36:2373–79). However, these studies were retrospective re-reviews of 4-phase studies, may have been confounded by memory bias, and did not address confidence in reporting lesions on 4D-CT, which can have a significant impact on a surgeon’s decision to perform MIP. At least 2 studies have argued that a 3-phase protocol is the optimum technique for confidently identifying parathyroid lesions preoperatively, based on prediction model performance11 and variability of parathyroid adenoma enhancement patterns, respectively.20 Anecdotally, a 3-phase protocol seems to be the current preferred approach at many large tertiary referral centers and has been described as a favored protocol in at least one “how to” review article.10
Multiphase imaging raises appropriate concerns regarding radiation exposure. Depending on the protocol, 4D-CT can have an effective dose more than twice that of scintigraphy, and is associated with a markedly higher organ dose to thyroid.17,18 4D-CT should be used judiciously in young patients.17 However, estimates of lifetime radiation-induced cancer incidence remain low, and the benefits of increased diagnostic accuracy of 4D-CT likely outweigh the very small attributable risk in the older population, keeping in mind that the average age of disease onset for primary hyperparathyroidism is in the fifth and sixth decades of life.1,18 4D-CT has also been shown to be more cost-effective than scintigraphy and, if used as a first-line imaging modality, may have the potential for lowering overall radiation dose and costs if additional imaging tests are avoided.1,18
Dynamic contrast-enhanced MR imaging has the potential to provide similar anatomic detail and perfusion characteristics to 4D-CT, but without ionizing radiation. In the past, MRI was unable to achieve adequate spatial and temporal resolution over the large FOV required for parathyroid imaging; however, a few recent studies have utilized fast imaging techniques such as time-resolved imaging with stochastic trajectories (TWIST) and new fat saturation techniques to overcome these technical limitations13 (AJNR 2015;36:2147–52). Although the sample sizes are small, the initial results are promising, with reported diagnostic accuracies and sensitivities equal to or greater than those reported for 4D-CT.12,14
In summary, the radiologist has much to offer the surgeon and patient contemplating MIP for primary hyperparathyroidism due to recent innovations in parathyroid imaging. 4D-CT combines excellent anatomic detail with perfusion data to provide high confidence for surgical planning,