Guest Editor |
 Guest Editor |
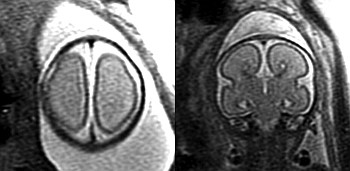
In the last years, the significant and continuous development of fetal MR imaging has revolutionized the prenatal diagnosis of congenital and acquired brain anomalies.1,2 In the early nineties, most diagnostic fetal MRI sequences were time-consuming and, hence, highly susceptible to fetal motion. Images of diagnostic quality could be achieved only by aggressive immobilization of the fetus, eg, by injection of curare into the umbilical cord prior to the study. Nowadays, ultrafast MR sequences allow for high-resolution anatomic and functional MRI images of the fetus without risk for the fetus and mother.
Prenatal ultrasonography (US) is widely accepted as the most important primary imaging modality to study the fetal brain. Prenatal US allows for the evaluation of the macroanatomy of the central nervous system.3 US is, however, limited for the detailed evaluation of the complex maturational processes involving the fetal brain, and subtle developmental or disruptive lesions may consequently be overlooked. Nonetheless, identification of all details of a fetal brain pathology is essential to making a reliable and specific diagnosis. A specific diagnosis is paramount for prognosis and counseling of the family. Therefore, alternative imaging techniques are occasionally necessary.
Fetal brain MRI evolved into an important second-line imaging tool to confirm, correct, or complete prenatal US diagnosis of complex pathologies of the fetal central nervous system. The most obvious finding may only be the tip of the iceberg. Agenesis of the corpus callosum may be associated with additional findings like abnormal gyral pattern as well as cerebellar and/or brain stem anomalies, which are less obvious on prenatal US.4 The identification of additional findings may allow a more specific diagnosis and may affect the long-term neurologic outcome. Nabavizadeh et al compared pre- and postnatal brain MRI findings in fetuses/children with schizencephaly and found that nearly half of prenatally open schizencephaly defects had closed on postnatal imaging.5 This observation has important implications for prenatal counseling because the prognosis of “open-lip” schizencephaly is known to be less favorable compared with “closed-lip” schizencephaly. Brossard-Racine et al compared 144 fetuses with congenital heart disease to 194 control fetuses and found that brain abnormalities such as ventriculomegaly and increased extra-axial spaces are present in 23% of the congenital heart disease group, compared with 1.5% in the control group.6 These findings demonstrate that brain abnormalities in this vulnerable population may occur already in the early fetal age.
Similar to “postnatal” neuroimaging, ongoing hardware and software developments in MR have allowed a shift in the imaging approach from an initially purely anatomic imaging (T1- and T2-weighted MRI sequences) towards a more advanced, functional data collection. Functional MRI nowadays includes diffusion-weighted (DWI) and diffusion tensor imaging (DTI), 1H MR spectroscopy (MRS), dynamic MRI, and resting-state functional MRI.7-9 These new developments have expanded our