Dystonia is a debilitating condition for which deep brain stimulation (DBS) has been suggested as an effective and minimally invasive therapy; however, experience with DBS for dystonia has been mixed. One of the major barriers with dystonia DBS is the lack of immediate clinical biofeedback, such as that seen with Parkinson disease and essential tremor. While these motor symptoms, such as tremor, often respond immediately to activation of DBS, dystonia treatment effect may take weeks or months to manifest, which makes both targeting and programming a much more difficult feat. During the surgical procedure, the lack of immediate biofeedback limits intraoperative testing for efficacy and may therefore result in a higher percentage of off-target implantations. Secondly, the postoperative programming is limited, as parameters generally must be blindly chosen and investigated for several weeks to determine whether modification is required. This leads to substantially longer intervals, on the order of months to years, to optimize programming for dystonia, if such optimization is ever reached. This model highlights a huge biomarker gap where connectomics is more needed than ever.
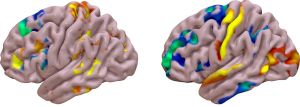
In this pioneering study of connectomics in dystonia DBS led by research fellow Lela Okromelidze, my team was the first to explore connectomics-driven outcomes in generalized dystonia to explore the potential feasibility of a connectomic biomarker to aid targeting and programming. Using a cohort of previously treated patients with dystonia, we analyzed the spatial “sweet spot” for optimal dystonia improvement and found this target to reside slightly more laterally than previously hypothesized along the globus pallidus internus (GPi)/globus pallidus externus (GPe) border posteriorly in the sensorimotor portion of both nuclei. This location suggests a potential role of the GPe efferent tracks to the GPi as a potential modulator for dystonia improvement. This was supported by our connectomic analysis, which confirmed that network overlap with the somatomotor network is a primary driver of improvement in dystonia. Since our publication, studies by other groups have subsequently produced similar results analyzing both generalized dystonia as well as cervical dystonia.1,2 Importantly, this pallidothalamic pathway may underlie a core feature of dystonia pathophysiology, as we would later discover in a separate study looking at dystonic tremor. In this subsequent study, we found additional benefit with stimulation of the ventralis oralis nucleus (site of pallidothalamic input into ventral thalamus) in patients with dystonic tremor compared with the more posterior ventral intermediate nucleus (traditional target for Parkinson tremor and essential tremor).3