Last year, ultra-high-field 7T MRI was approved by the FDA and the European Union for clinical use in routine daily practice. The scientific community has great expectations from this technology, on the one hand due to the high spatial resolution that can be achieved and, on the other hand, due to the much-improved visualization of paramagnetic substances on susceptibility sequences.
Which organs will benefit most from this type of imaging?
Definitely the brain, due to its anatomic configuration and the fact that it is a near-motionless organ. Furthermore, the brain also allows all types of advanced imaging such as DTI, functional imaging,1 and spectroscopy.2 Conversely, 7T spine imaging is still in its early stages and requires more time and coil development so as to improve signal-to-noise ratio and decrease artifacts in order to achieve the same image quality as 3T MRI.
Several questions may arise concerning this type of MR scanner: Is it easily applicable in a clinical setting? Which patients will be eligible to be scanned at 7T? What are the side effects? Which clinical indications are appropriate—all indications or only for patients who previously underwent 3T MRI that failed to answer the clinical question? Will we need to learn a new neuroradiologic semiology?
At present, the clinical indications that seem to benefit most from this type of imaging are epilepsy,1,3,4 aneurysms,5 multiple sclerosis,6 ischemia,7 arterial wall imaging,8 cavernomas,9 and dementia.10
The most common side effects seem to be vertigo, flashing lights, and a metallic taste in the mouth.
Currently, some clinical papers concerning hot topics in neuroradiologic imaging are starting to appear in specialized literature.
There are great expectations for 7T MRI concerning advances in new semiology, in the understanding of histopathologic mechanisms, and in detecting new findings, which may improve diagnostic accuracy and therefore change treatment and prognosis of some conditions.
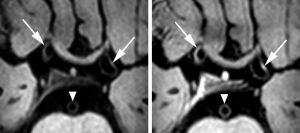
New imaging signs are emerging and facilitating the detection and diagnosis of different pathologies such as the intracortical black line sign in type IIb focal cortical dysplasia,11 vascular distribution in polymicrogyria, venous structures associated with tubers in tuberous sclerosis complex,3,4 venous angioarchitecture of cerebral cavernous malformations,9,12 or concentric enhancing foci of the ipsilateral vessel wall to the treated artery after thrombosuction8 compared with the contralateral side.
What is the reality?
7T MR imaging requires highly specialized engineering support in order to optimize the sequences, as well as to understand and minimize artifacts. Currently, this type of scanner is almost entirely reserved for research settings and cannot be found in hospitals, nor is it used in daily clinical practice. This makes it difficult for patients to access this technology and most of the research is carried out on volunteers and selected patients. Despite the current situation, we expect that this type of imaging will soar when 7T MR scanners are installed in university hospitals.
As opposed to MR scanners at lower magnetic field strengths, 7T MRI will allow clinical and functional protocols to coexist in harmony and intertwine, which should result in faster and more effective imaging.13
Limitations
Limitations of 7T MRI relate mainly to long image acquisition time, elevated specific absorption rate (SAR)—particularly in spin-echo‐based sequences, which limits the number of slices—and also issues relating to metallic devices and artifacts.
The first limitation could be overcome by using multiarray coils in combination with parallel imaging. Decreased SAR could be achieved with the implementation of adiabatic pulses and lower flip angles.
There are only a few metallic devices that have been tested with this type of scanner, and there are still many more that need testing for 7T compatibility.14
Artifacts of inhomogeneity are mostly seen on 3D FLAIR and DWI. Issues of geometric distortion and loss of signal, particularly at the level of the cerebellum and temporal lobes, have been almost completely resolved with the use of dielectric pads.