Our Search for Evidence of Impaired CSF Homeostasis in Obesity-Associated Idiopathic Intracranial Hypertension
Noam Alperin
The CSF system is a fascinating, elegant biomechanical environment important for a wide range of critical physiologic processes, from facilitating the cerebral circulation of the pulsatile blood flow in the confined space of the cranium to the accommodation of large hydrostatic changes that occur following a change in body posture (eg, supine to upright). My interest in idiopathic intracranial hypertension (IIH) is integral to my longstanding research focus on the CSF system in the health and disease states.1 Early on in our research, it became evident that IIH is not a single etiology. While at the University of Illinois at Chicago, we studied with MRI a heterogeneous group of patients, including slim children and adolescent patients, with or without visual impairments. Our first reported observation was the involvement of the extracranial venous drainage pathways in the pathophysiology of IIH.2 Prior to this work, clinical and research focus was primarily on the intracranial venous sinuses. After relocating to the University of Miami, I was fortunate to meet and collaborate closely with Dr. Byron Lam, MD, an outstanding clinician and researcher from the Bascom Palmer Eye Institute with similar interest in IIH, and Drs. Sklar and Lavi, experienced neuroradiologists in our department. Together we initiated a multidisciplinary team focused on the investigation of the more typical type of IIH, obesity-related IIH in women of childbearing age. The approach of comprehensive multimodal quantitative characterization of the symptomatology, visual and ocular changes, brain anatomy, and the cerebral hemodynamics and hydrodynamics, from the pretreatment through the treatment phases, provided a great dividend of new insights and understanding.3–7
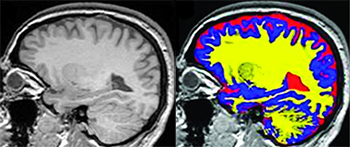
For example, quantitation of the intracranial CSF volume in a cohort of pretreated female patients with obesity and IIH and a BMI- and age-matched cohort of healthy female subjects revealed a significantly larger intracranial CSF volume in IIH. Notably, the increased amount of CSF accumulates in the extraventricular spaces while the ventricles are normal in size. Apparently, radiologists often rely on inspection of the ventricles for an indication of changes in CSF spaces, thereby not realizing the enlarged intracranial CSF spaces in IIH. This finding should serve as a reminder to neuroradiologists that some tasks are done more reliably by computational analysis, and now is the time to start incorporating unbiased quantitative measures into radiologic reporting.