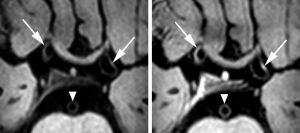
Our university hospital has a dedicated research department focused on both research and clinical applications of 7T MRI. One of our clinical studies is the Intracranial Vessel Wall MR Imaging (IVI) study, a recently completed cross-sectional study that over the past 10 years has included patients with acute ischemic stroke or transient ischemic attack for dedicated intracranial vessel wall MRI at 7T. While evaluating the intracranial arterial vessel walls of these patients for possible vessel wall lesions, we noticed that some of the patients had striking unilateral (and often concentric) enhancing vessel wall thickening, which seemed to be mainly present in stroke patients treated with intra-arterial thrombectomy. This led us to hypothesize that this procedure may cause transient or perhaps even permanent intracranial vessel wall changes, which could be visualized using 7T vessel wall MRI.
Intra-arterial thrombectomy (IAT) is a minimally invasive interventional procedure currently available for patients presenting with acute ischemic stroke and a proximal intracranial arterial occlusion. In these patients, the occluded artery is reopened by means of mechanical thrombectomy using either a stent retriever or thrombosuction device, or both. If successful, it restores blood flow to the affected brain parenchyma, increasing the chance of neurologic recovery. There is some evidence that IAT may affect the intracranial vessel wall, but limited in vivo MR imaging studies are available, especially on the effects of thrombosuction devices in IAT, which are the mainstay in our center. To investigate whether IAT by means of thrombosuction causes vessel wall damage, vessel wall enhancement of IVI study participants was compared between those who received IAT (IAT group) and those who did not (non-IAT group).