Didier Dormont
Deep brain stimulation (DBS) was initially employed to cure intractable tremor in the early 1990s1 by A. Benabid, a French mathematician and stereotactic neurosurgeon who, at that time, described bilateral subthalamic nucleus DBS for advanced Parkinson disease (PD).2 Coubes in Montpellier3 utilized chronic bilateral stimulation of the internal globus pallidus to cure generalized dystonia. In the United States, the Food and Drug Administration approved DBS for essential tremor in 1997, for PD in 2002, and for dystonia in 2003. In 2013, more than 100,000 patients worldwide have been treated with DBS.
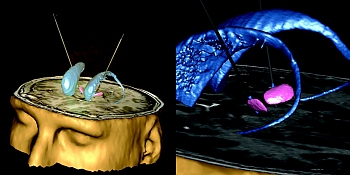
At the Pitié-Salpêtrière Hospital in Paris we have worked on brain imaging for DBS since the early 1990s. Early investigators used primitive ventriculography to identify targeted nuclei indirectly. We developed modern MRI-based techniques and have improved the accuracy of stereotactic MRI through direct visualization of the targeted structures, achieving accuracy to the level of one pixel.4 We used MR to implant DBS electrodes to treat patients with essential tremor.5
All DBS procedures in our center are performed using MR guidance. We have also worked on the identification of the subthalamic nucleus in MRI6 and since the beginning of 2000s, we have developed a new 3D atlas of the basal ganglia with J. Yelnik and E. Bardinet.7 Our work in neuroradiology has led to the publication of numerous articles, in collaboration with teams from neuroscience and neurosurgery, on the results of DBS in PD and also in obsessive-compulsive disorders, dystonia, and Tourette disease. The combination of MRI identification of nuclei with the 3D atlas of the basal ganglia developed facilitated fundamental discoveries on the role of the basal ganglia in patients treated with DBS.
The review article published by AJNR in 2010 on neuroimaging and DBS8 summarized worldwide progress since the first description of DBS. We reviewed the use of brain imaging for patient selection, target nucleus localization, postoperative complications detection, and final electrode contact selection. Our experience and reports in the literature demonstrate that that active neuroradiologist involvement in these procedures is critical to their success. A multidisciplinary approach is