Sotirios Bisdas
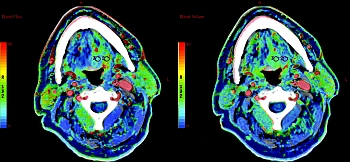
Malignancies in the head and neck and their nodal involvement often present in an advanced stage that reduces the chances for successful treatment and prolonged survival rates. Though clinical endoscopic examination is the cornerstone of therapeutic strategies, follow-up is hampered by unspecific tissue changes, whereas the response on the increasingly used neo-adjuvant therapy regimens is often inadequately assessed by conventional CT and MR imaging. Perfusion imaging, which visualizes the tissue pathophysiology, is mandatory in order to monitor the disease during and after the completion of organ-preserving radio(chemo)therapy and, thus, prompt accurately timed treatment tailoring prior to any delayed morphologic changes. Long-term retrospective survival studies of patients undergoing standardized operative treatment followed by radio(chemo)therapy are also important, because the baseline perfusion values have evidence-based predictive and prognostic value and may trigger individualized radiotherapy principles in the future. These fundamental conceptual changes of treatment planning are required for the move to individualized medicine, and thus, perfusion CT and MRI receive increasing acceptance among radiologists worldwide. This is also reflected in the numerous PubMed entries, as well as in the international meetings, where perfusion imaging is a “hot topic” and is extensively debated.