Varallyay P, Nesbit G, Muldoon LL, et al. Comparison of Two Superparamagnetic Viral-Sized Iron Oxide Particles Ferumoxides and Ferumoxtran-10 with a Gadolinium Chelate in Imaging Intracranial Tumors. AJNR Am J Neuroradiol 2002;23:510–19

Seymur Gahramanov
This early clinical paper compared 2 different iron oxide nanoparticle contrast agents with gadolinium-based contrast agents (GBCA) using standard MRI sequences to assess anatomic characteristics of intracerebral neoplasms including location, size, and extent.
Different central nervous system pathologies can appear to be similar anatomically on MRI. GBCA-contrast-enhanced T1-weighted MRI represents information regarding the integrity of the blood-brain barrier, rather than the physiology of the brain lesions. Therefore, noninvasive imaging tools to assess pathophysiologic characteristics of CNS lesions are desirable. I am particularly interested in tumor angiogenesis assessment due to my neurosurgery/neuro-oncology background. Angiogenesis is one of the key elements of tumor growth and the target of multiple newly developed medications, yet it cannot be assessed just by using anatomic MRI sequences. Cerebral blood volume (CBV) measurement by perfusion-weighted MRI allows noninvasive measurement of tumor angiogenesis. Accurate CBV measurement using a standard dynamic susceptibility contrast MRI modeling approach relies on intravascular localization of contrast agent in the tissue of interest. This condition is compromised by the leaky BBB present within malignant brain tumors, especially after radiation and chemotherapy. Rapid extravasation of standard GBCA from blood vessels into the extravascular/extracellular space can lead to underestimation of CBV. To improve the diagnostic accuracy of DSC MRI with GBCA, several methods have been proposed for leakage correction, such as the use of small flip-angle gradient-echo or dual-echo perfusion acquisitions, contrast preload methods, or postprocessing with multiple mathematic correction algorithms, but these still have a lack of consistency and reproducibility, and depend on magnetic field strength differences and MR pulse sequence details. Ferumoxytol iron oxide nanoparticles are confined to the blood pool for several hours after IV administration. The absence of ferumoxytol extravasation during DSC acquisition greatly simplifies modeling and evaluation of tumor angiogenesis.
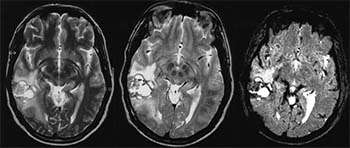
Figure 1. Evaluation of the effect of antiangiogenic therapy on tumor relative cerebral blood volume (rCBV) measured using gadodiamide (Gd) versus ferumoxytol (Fe). Anatomic T1WI with contrast medium (T1W+CM) shows tumor enhancement with Gd but not with Fe. Decrease of T2 signal and Gd-enhancement after treatment is apparent. Tumor rCBV is variable between no preload, single-dose (s.d. preload), and double-dose (d.d. preload) contrast preload when Gd is used, while, with Fe, rCBV is consistent regardless of preload dose. Note, both contrast agents showed that bevacizumab treatment decreased rCBV. Reprinted with permission from Gahramanov et al, Radiology 2011.1