Guest Editor |
 Guest Editor |
Increased accessibility and improved image quality have increased the use of medical imaging, particularly in emergency departments.1,2 However, with the rising medical costs and burden on the health care system, it is the impetus of the health care community to be cognizant of resource allocation in order to reduce waste. Imaging is critical for the evaluation of a patient with spine trauma. The most accurate and cost-effective imaging modality for detecting fractures is multidetector CT (MDCT). The study by Griffith et al demonstrates that strict application of clinical guidelines, such as the National Emergency X-Radiography Utilization Study Low-Risk Criteria3 and Canadian Cervical Spine Rule,4 would enable the appropriate utilization of screening CT for blunt trauma, allowing for decreased radiation exposure and improved resource use.
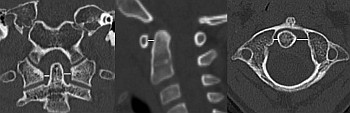
With increased use of MDCT, investigators have reevaluated previous plain radiography imaging parameters that have been used to assess cervical spine injury.5,6 Recent articles report objective CT criteria to indicate spine trauma. Alhilali and Fakhran determined that an intervertebral disc angle greater than 13 degrees is suspicious for anterior discoligamentous injury, warranting further evaluation with MRI, and that greater than 18 degrees is always associated with such an injury.7 They found this more accurate than subjective assessment of disc widening and important to evaluate, given that occult discoligamentous injury is seen in up to 44% of patients with persistent midline tenderness despite their having had a negative CT.8 Additionally, recognizing normal CT appearances in different age groups is important in order to avoid unnecessary work-up, which may result in increased radiation exposure, testing (ie, MRI), and prolonged stabilization in the cervical collar. Eran et al found that odontoid lateral mass asymmetry can be a normal finding in those pediatric patients without cervical tenderness and with a normal atlantodental interval.9 Pediatric patients are particularly vulnerable to craniovertebral injuries due to the morphology and biomechanics of this region. Meoded et al eloquently describe the CT and MRI features of tectorial injury in children resulting in retroclival epidural hematoma.10 MRI may show overt ligamentous disruption; however, there may be indirect signs in more subtle cases (eg, stretching, fluid collection extending to the dens apex).
MRI has a complementary role in spine trauma evaluation when there is concern of ligamentous, cord, and vascular injury and for the delineation of epidural hemorrhage. MRI pattern of injury can be used in clinical decision-making by determining ligamentous instability and can be used for the prognostication of acute spinal cord injury.11 MRI has high sensitivity for detection of ligamentous injury but has a low specificity for correlative intraoperative findings of disruption.12,13 Martinez-Pérez et al, however, showed that detection of ligamentous injury (particularly the ligamentum flavum) correlates with spinal cord lesion length. In this way, they attest that it may be useful in predicting neurologic outcome. They also examined the general recommendation that MRI be performed 24–72 hours after injury15 due to the dynamic nature of intramedullary edema and dependence on lesion length,16 as the subjects in their study underwent MRI within 96 hours of injury, reasoning that soft-tissue injury is static and that acutely unstable patients may not be able to undergo MRI sooner.
MRI is not without limitations. Due to the longer acquisition times and susceptibility to artifact, the percentage of highly diagnostic MR imaging studies may be lower compared with CT studies.10 It is relied upon that fluid-sensitive sequences (eg, short tau inversion recovery [STIR], T2WI with fat saturation) can detect marrow edema of acute fractures. Lehman et al (not discussed in this edition) demonstrated an association between the prevalence and degree of facet joint signal abnormality with acute/subacute lumbar compression fractures.17 However, the reliability of MRI in determining the acuity of fractures has been raised by recent